Welcome to the dermatology rotation
During this rotation you will work at Dr. Petit’s office and at the VA Dermatology Clinic supervised by UC Dermatologist. Dermatology complaints are very common in the outpatient office and this month can go a long way to improve your comfort in diagnosis and treatment of common complaints. To meet your goals for the month requires not only working with the dermatologist, but also significant outside reading and study. To assist in this, below you will find required asynchronous learning modules you are to complete during the month. It is strongly recommended to complete these earlier in the month so you can practice and hone your skills through your time with the dermatologist. In addition to the learning modules, the website also has an excellent overivew of the Skin exam. Please be sure to review the goals and objectives for the month along with reviewing the procedure curriculum for those procedures you are expected to obtain during this month.
Enjoy your month!

Required Learning Modules
The American Academy of Dermatology has developed outstanding learning modules on core dermatology topics. Over the course of your month, please complete the below topics, starting with the Normal Skin Exam. It is strongly recommended to complete these in the first two weeks of the month, as you will find your time with the dermatologist more valuable the more prepared you are. Each learning module has slides to review, videos, and then a quiz.
Complete the following: (Note: You will be required to create a login the first time you access the modules. This is free. After you create the login, return to this patient and access the modules directly from the below links. The webpage can be quite slow in downloading the first time, but after the first time, it will speed up)
Learning Modules
The Skin Exam (Do not need to see all of the videos)
Procedure Videos (Not required; recommended to review)
Articles
Introduction to the Skin Exam
Dermatological diagnoses are made from three elements, the history, the physical examination and at times with the assistance of laboratory data. There are thousands of different dermatological abnormalities. Most physicians cannot memorize all these disorders. Rather they must learn to categorize disorders so that they can refer to textbooks for help in finding the proper references where information about the disorder, its evaluation, work up and treatment are available.
To categorize the disease we use the physical examination. The history tells us less about the precise category to which a disorder belongs than about general features of the disease. We can tell that a person has a dermatitis (inflammation of the epidermis) only from the examination of the skin. The history gives US critical clues as to the cause of the dermatitis such as contact allergens, irritants, genetics from family history. History will help us decide if we can cure the disease. Genetic disorders and many metabolic disorders are not curable. Disorders like albinism or ichthyosis are not curable and usually are present at birth. Generally there is a history of others in the kinship who have the same problem. Disorders that have been present for many years usually are not curable like psoriasis or atopic dermatitis. In contrast, allergic contact dermatitis (poison ivy or allergies to other chemicals) are usually curable by avoidance of the allergen. The history will often pinpoint the allergen.
On the physical examination we must learn about the type(s) of primary lesions, their location and distribution, and their life history. The lesions usually will be identifiable as new, older and involuting or old lesions. Thus we can ascertain what the eruption looks like when it begins, at its zenith and when it heals. We can see the entire biological profile of the eruption. These features help us categorize diseases.
When examining a lesion you must determine which of the three layers of the skin is affected, the epidermis, the dermis or subcutaneous fat (or several of these layers). You must also ask yourself what cells, tissues, fibers or other elements are involved. To do that you must know of the constituents that compose each layer of the skin.
The epidermis is composed of keratinocytes, melanocytes and Langerhans cells. The dermis has the capillaries, the fibroblasts, the collagen, elastic tissue, Iymphocytes, nerves and other elements. The subcutaneous fat is mostly composed of lipocytes, fibroblasts and blood vessels.
A list of primary and secondary lesions and schematic drawings of their histology is included for your study.
When examining a lesion first determine what type of primary lesion it is. Next ask what is the significance of the lesion. Some have great import for the patient, others have no significance other than curiosity or cosmesis. If a cell or tissue is affected in the skin, consider whether the same tissue is affected in another organ. For example, vasculitis on the legs often is the signal of vasculitis in the kidneys, brain and other organs. A nevus flammeus on the foot has little known significance. A nevus flammeus on the face, especially the forehead, is often a sign of a similar vascular malformation in the leptomeninges (Sturge Weber syndrome). These individuals will have seizures and often are mentally retarded.
MACULES

Macules are color changes. By definition a macule is flat. It is visible but not palpable. Each color change represents some abnormality in the epidermis, dermis or subcutaneous fat. Color usually denotes some biological process. Learn what a color means. It permits you to interpret what you are seeing.
White macules: The skin gets its color mostly from melanocytes. So white discoloration usually (but not always) represents some abnormality of the melanocyte. Hypopigmentation or partial loss of pigment usually represents a dysfunction of the melanocyte. The cells are present but not functioning to 100% of capacity. An example is pityriasis (scaling) alba (white). Depigmentation or total loss of pigment usually represents loss of melanocytes. Examples are vitiligo.
Brown macules: Brown suggests the presence of melanin which is synthesized by the melanocyte. That the lesion is macular suggests that the melanocyte has not proliferated but is making excessive melanin. Examples are cafe au lait macules.
Blue macules: Blood in the dermis and subQ can appear blue. But in general blue means that there is some DARK substance or dark cells In the dermis. Anything that is dark that gets into the dermis has a blue appearance. That can be a foreign body like dirt caused by an abrasion. It can be a tattoo or gun powder. These are substances that penetrate the skin, one route of entry. Dark substances can be endogenous. It can be melanin or melanocytes in the dermis. It can also be a melanoma. Or dark substances can enter the body by ingestion. Medications like minocycline are notorious for causing skin problems.
Red macules: The only tissue in the skin that is red is capillaries. Dilated capillaries cause erythema on the skin. Erythema can be caused by several processes. It can be caused by inflammation and then should have the other features of inflammation (red, hot swollen, tender). Erythema can be caused by developmental defects like the nevus flammeus. The nevus flammeus is an anomaly due to dilatation. They should not be called an hemangioma. Hemangiomas are proliferations of vessels (space occupying) and produce papules or nodules.
Yellow macules: Yellow usually means lipid unless the entire body is yellow and that suggests jaundice. Localized accumulations of lipid cause yellow macules. Yellow lipid can accumulate from ingestion of excessive amounts of beta carotene (the yellow dye that makes margarine look like butter) or from endogenous lipids. You must ask yourself why does lipid accumulate in the skin? Is it from an endogenous or exogenous cause? Do you need to be concerned about the etiology of the lipid deposition?
PAPULES, NODULES AND TUMORS

Papules are small 15 mm raised lesions. They are always palpable. Nodules are larger, usually 5 mm or larger. Tumors are larger still. Determine the size or range of sizes of the lesions, i.e., 2 10 mm papules and nodules. Of course these lesions also have a color. Specify if the lesion is normal color, pink, brown, etc. For the lesion to be raised, it must have some space occupying substance or cells.
White papules: Small white papules can represent an unusual form of inflammation like lichen nitidus or sometimes small scars. They are not common.
Brown papules: These suggest the presence of melanin. What in the skin makes a brown pigment? The papule suggests the presence of space occupying cells and that the melanocytes have proliferated and are making melanin but that the process is confined to the epidermis because it is brown. A nevus making pigment in the dermis would appear blue.
Blue papules: Blue represents something dark in the dermis. It can be a foreign body like gun powder. It can be endogenous and benign like a blue nevus. These are normal melanocytes that are in the dermis where they make melanin. A blue nodule or papule can also represent a malignant melanocyte or melanoma. The lesions represent melanin producing cells in the dermis.
Red papules: Red represents either vessels or inflammation. Vessels are proliferations of capillaries and are called hemangiomas or angiomas. In contrast inflammation represents infiltration of mononuclear cells with vasodilation and edema (inflammation is defined as a red, warm, swollen, tender area). Infants often have hemangiomas. Sometimes they are very large and called tumors. The word tumor does not imply malignancy but rather size. Inflammatory papules and nodules can be caused by many things such as infections from bacteria, viruses, fungi and many other causes. The dermis can be infiltrated also by benign Iymphocytes of non-infectious origin or malignant Iymphocytes (a Iymphoma or in the skin, mycosis fungoides).
Yellow papules: Yellow is lipid. Sometimes the accumulation of lipid occupies sufficient space to cause a raised lesion. Eruptive xanthomas are an example.
Skin colored papules: Fatty cells, nerves, collagen, elastic tissue and other elements can fill the dermis and produce a papule that has the color of the surrounding skin. Fat has a certain feel on palpation as does neurofibromas, collagen and elastic tissue.
Nodules:

These are larger papules, usually 1 cm in size. They represent the same processes as papules. Often a rash is composed of papules and nodules that have a color.
Tumors:

Usually the term tumor is reserved for a large mass. Tumors can be large nodules and have the features described above. But sometimes tumors have other features such as ulceration. You must ask why a lesion is ulcerated. Trauma is common but should be transient. The lesion should heal if it has been mechanically injured. Some tumors ulcerate easily and remain ulcerated. That is called being friable or subject to injury. Certain biological processes make tumors friable. For example cancers are friable and ulcerate for two reasons. They tend to outgrow their blood supply and therefore some of the cells die. The tumor has a necrotic area and that ulcerates. But tumors also destroy the integrity of the skin. Recall that the skin is very strong; it has remarkable tensile and elastic strength. Thus we can run, stop, twist and our skin does not get ripped off (unless you have a genetic disorder that interferes with the construction of the skin such as Ehlers-Danlos syndrome). But tumors destroy the structures that keep the epidermis and dermis intact. Thus basal cell, squamous cell carcinoma and melanomas all ulcerate. Metastatic tumors also destroy the structures of the skin making it friable. Thus ulceration is often a sign of malignancy.
VESICLES AND BULLAE (and pustules)
This group of lesions is filled with fluid that is clear or purulent. Vesicles are small lesions, usually less than 5 mm in diameter. Bullae are larger. Rather than worry about the precise term, give a measurement. "There are 2-10 mm vesicles and bullae scattered over the patient's body.” Vesicles and bullae can be located in the epidermis or below the epidermis. The most superficial are below the stratum corneum and are observed in impetigo. Poison ivy or other forms of allergic contact dermatitis are located in the middle of the epidermis. The blisters of bullous pemphigoid are beneath at the membrane of the basilar keratinocytes. The blisters of toxic epidermal necrolysis are through the basilar keratinocytes. Some disorders are within the basal lamina that is immediately below the basilar layer. Disorders can be characterized by their location. Remember that intraepidermal blisters do not bleed because the capillaries are in the dermis. Those blisters in the basal lamina are close to the capillaries and tend to bleed. Pustules are fluid filled lesions containing pus which has a white, yellow or green color.
Vesicles:

These are small and fluid filled. If grouped they suggest herpes simplex. If present in a dermatomal pattern, they suggest herpes zoster (chicken pox). They are usually filled with clear fluid early in the course of the disease, but with pus (pustule) later in the course.
Bullae:
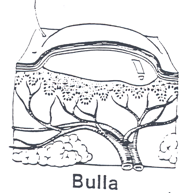
These are larger fluid filled lesions. Examples are bullous pemphigoid, pemphigus, poison ivy or other forms of contact dermatitis or the bullae of diabetes.
Pustules:

Purulent fluid in a lesion.
WHEALS

These are welts. The lesions are raised and palpable and usually erythematous suggesting increased blood flow. Examples are hives. Sometimes they are not red but can be whitish due to decreased blood flow. Examples are cold urticaria or cold induced hives. A raised plaque always indicates some space occupying substance, cells or tissue. Urticaria is caused by leakage of serum and other fluids from the capillaries into the dermis. The red cells are retained within the vascular system. (Compare to capillaritis with extravasation of red cells without fluid and to vasculitis that is manifested by extravasation of red cells and fluid.)
The diagnosis of hives (urticaria) is not difficult. Identifying the cause of urticaria is usually very difficult.
PURPURA
Purpura is a discoloration of the skin due to extravasation of the blood from within the capillaries into the surrounding dermis. Shortly after the extravasation, the blood will be red and the lesions bright red. As the cells lose their oxygen, the lesions become a blue to purple color. Later only the iron persists in an oxidized state. (Ferric iron is rust and skin with ferric ions is technically rusty). We call it hemosiderin.
Petechiae: These are small and can be macular. A common cause is inflammation of the capillaries. This is called capillaritis. It is common. The petechiae evolve through the red to purple to orange state. The infiltrate around the capillaries is Iymphocytic and does not injure the capillaries or cause the serum to extravasate.
Petechiae also can be raised. That indicates some space occupying substance. Raised purpura is also called palpable purpura and indicates that the capillaries are damaged and leaking both fluid and red cells. The usual cause of palpable purpura is immune complex vasculitis. Immune complexes composed of antigenantibody complexes deposit in the capillaries and attract neutrophils that destroy the capillaries. The blood and serum extravasate. Often the skin is a manifestation of a similar process in the kidneys, intestine or brain.
Ecchymoses: These are large hemorrhagic macules or plaques. They can be a manifestation of injury (a bruise) or a metabolic condition like vasculitis. Thrombocytopenia is a cause of bleeding into the skin.
Hematoma: A collection of blood in the tissue. It Is raised.
SECONDARY LESIONS
Scaling: The presence of scale suggests that the stratum corneum is not forming the corneocytes normally, that is, the process of keratinization is abnormal. Keratinization can be abnormal for many reasons. The process can be altered by mutations. These are present from birth and the most common causes are the forms of ichthyosis. The process can be altered by metabolic forces. For example, psoriasis is a metabolic abnormality of the keratinization process. It tends to run in families but is not an obvious genetic disorder. Keratinization can be altered by inflammation, so that those with chronic inflammation of the epidermis develop scaling. Inflammation of the epidermis is called dermatitis (a better name would be epidermatitis). Usually an acute, short lived dermatitis causes no scaling. But if it persists for a week or two, then scaling develops. Atopic dermatitis persists for years and is usually manifested by scaling.
Crusts: Crusts indicate dried serum. Crusty skin and scaly skin are not the same. The former indicates that serum has exuded from a lesion, the latter that the keratinization is abnormal. Impetigo, an infection of the skin by staph aureus, commonly presents with yellow crusts. Sometimes both processes can be observed together. Nummular eczema (eczema is a type of chronic dermatitis) is an inflammatory process that oozes fluid that congeals and produces yellow crusts. But it is not caused by staph. It persists for years and like all dermatitis eventually results in scaling. Hemorrhagic crusts indicate bleeding into the fluid.
Erosions: These are superficial disruptions or loss of the epidermis. Usually erosions are loss of several layers of epidermis. Staph scaled skin syndrome is a classical example.
Ulcers: A deep loss of skin, usually into the dermis. An abrasion from falling on the sidewalk, a decubitus ulcer are examples.
Excoriation: A longitudinal erosion or ulcer caused by scratching with the nails or some object such as a stick, knifes or other object.
Fissure: A longitudinal split in the skin.
Atrophy: A thinning or wasting of a part or all of the skin. The skin has three layers, the epidermis, the dermis and subcutaneous tissue. One or all of these layers can be atrophic. Usually loss of one cell or one structure does not cause atrophy. Thus in vitiligo there is complete loss of the melanocyte but we do not call the epidermis atrophic. The thickness of the stratum corneum and epidermis must be less than normal. Examples are actinic keratoses in which the epidermis has been damaged by the sun and is much thinner than normal. The dermis also can be thinner than normal due to loss of collagen. The most common cause is age. The subcutaneous fat also can be lost from inflammation or injections. Or the entire skin can be atrophic such as seen in Werner's syndrome, a rare dermatoses that causes loss of many elements in the three layers of the skin.